Fagfellevurdert
Essentials for sustainable physiotherapy: Introducing environmental reasoning into physiotherapy clinical decision-making
Fagartikkel
Filip Maric, Ph.D., Lecturer, Physiotherapy studies, Department of Health and Care Sciences, UiT The Arctic University of Norway. filip.maric@uit.no.
Karen Synne Groven, Ph.D., Professor, Oslo Metropolitan University & VID Specialized University.
Srishti Banerjee, Master's of physiotherapy, Assistant Professor, LJ Institute of Physiotherapy.
Tone Dahl Michelsen, Ph.D., Associate Professor, Oslo Metropolitan University.
This article ("fagartikkel") has been peer-reviewed according to Fysioterapeuten’s guidelines, and was accepted on 4 March 2021. No conflicts of interest stated.
Abstract
Introduction: Global environmental changes require the provision of sustainable health care and the decisive inclusion of sustainability considerations into all aspects of health care professional practice. In this article we illuminate how environmental sustainability might be positioned in physiotherapy and how environmental reasoning can inform future clinical reasoning in physiotherapy practice.
Main part: Environmental sustainability in physiotherapy relates to a two folded mandate of sustainable healthcare: to improve the sustainability of health care systems and services and contribute to the broader societal transition to sustainable futures. We suggest that measuring the environmental footprint of physiotherapy interventions should become a regular element of physiotherapy intervention research. This will enable the inclusion of an environmental layer to clinical reasoning in physiotherapy that we term environmental reasoning: The ability to include environmental sustainability considerations - based on relevant evidence of the environmental impact of physiotherapy services - into the collaborative clinical decision-making process shared by therapists and patients.
Conclusion: In this article we indicate a key pathway for introducing environmental sustainability into clinical decision-making via the measurement of physiotherapy intervention environmental footprint. This suggests an extensive research agenda with much to be explored, clarified and adapted as the physiotherapy profession makes first advances toward the inclusion and implementation of sustainability considerations.
Key words: environmental sustainability, clinical reasoning, physiotherapy.
Sammendrag
Betingelser for bærekraftig fysioterapi: Introduksjon av miljøresonnering i kliniske beslutninger i fysioterapi
Introduksjon: På grunn av globale miljøendringer trengs et bærekraftig helsevesen der hensynet til bærekraft gjennomsyrer alle deler av den helsefaglige praksisen. I denne artikkelen belyser vi hvordan bærekraft kan inkluderes i fysioterapi, og hvordan miljøresonnering knyttet til bærekraft kan inkluderes i fremtidens kliniske resonnering i fysioterapi.
Hoveddel: Miljømessig bærekraft i fysioterapi er knyttet til et todelt mandat for en bærekraftig helsetjeneste: å forbedre bærekraften i helsevesenets tjenester og systemer og bidra til den bredere samfunnsmessige overgangen til en bærekraftig fremtid. Vi foreslår at måling av miljømessige fotavtrykk integreres i all intervensjonsforskning innen fysioterapi. Dette vil legge til rette for et eksplisitt miljøfokus i klinisk resonnering; som vi betegner miljømessig resonnering: Evnen til å inkludere bærekraftshensyn – basert på relevant kunnskap om miljøpåvirkningen knyttet til fysioterapitjenester – i en klinisk beslutningsprosess, der både terapeut og pasient er medvirkende.
Avslutning: I denne artikkelen foreslås en konkret tilnærming for å innføre bærekraftstenkning i klinisk beslutningstaking gjennom måling av miljømessige fotavtrykk fra fysioterapiintervensjoner. Dette fordrer en forskningsagenda der mye må utforskes, avklares og tilpasses når fysioterapiprofesjonen tar viktige fremskritt mot inkludering og implementering av bærekraftshensyn.
Nøkkelord: miljømessig bærekraft, klinisk resonnering, fysioterapi
Introduction
Climate change, biodiversity loss, the disruption of biogeochemical cycles, air, water and plastic pollution and the widespread degradation of land and sea are fundamentally changing the environmental conditions that support human life on earth (1). The destruction of our global natural environment has been recognised as the largest threat to human health and flourishing in the 21st century and is already affecting the health of people around the world. Recognised health impacts expected to increase over the coming years include non-communicable disease, exposure to infectious and vector-borne disease, threats to human nutrition and food crops, as well as mental and physical trauma and injury due to extreme weather events, climate migration and other environment- and resource-related displacement and conflicts (2).
In light of the ubiquity and severity of todays interconnected environmental and health crises, it has been recognised that addressing them means working towards more sustainable futures and requires resolute action across all sectors of society, from multi-national endeavours to individual action in daily life. This is clearly stated in the UN Agenda 2030 Sustainable Development Goals (SDGs) explicit call for the ‘mobilisation of all available resources, participation of all countries, all stakeholders and all people’ and many other resonant publications (3).
For the health care professions, this represents a clear call for the inclusion of sustainability considerations into all aspects of professional practice, research and education (4,5). Looking towards clinical practice in particular, clinical reasoning has been a cornerstone of physiotherapy for the last few decades and is deeply embedded in physiotherapy education and practice (6). As a complex and multidimensional phenomenon involving problem solving and professional judgment, clinical reasoning combines the cognitive process of the physiotherapist and a narrative process that includes patients and others such as family and other healthcare practitioners (7). Rather than linear, clinical reasoning has been visualized as circular or spiralling, taking into account the interactive process between patient and therapist in the clinical encounter (8). What has been lacking so far, however, is a better understanding of how considerations of environmental sustainability must and can be included in clinical reasoning. We consider this indispensable in a world in which health can no longer be ensured effectively without simultaneously addressing the environmental conditions it is predicated on.
Aim
The aim of this article is to illuminate how the need for sustainability in future physiotherapy can be addressed by advancing the evolution of clinical reasoning. We address the following questions: How does sustainability relate to physiotherapy? In what ways can environmental reasoning inform future clinical reasoning in physiotherapy practice?
Main part
Sustainability in healthcare
In addition to the extrinsic imperative to include sustainability into health care as a central concern due to the health impacts of global environmental degradation, there is a compounding, intrinsic imperative resulting from healthcare’s very own contribution to environmental degradation and resulting ill health. A recent study of healthcare’s carbon footprint identified that ‘if the global health care were a country, it would be the fifth-largest emitter’ of greenhouse gas emissions of the world (9). Further adding to these significant carbon emissions, the healthcare sector is a significant producer of waste, air and plastic pollution, and uses extensive natural resources for transport and the development and provision of specialist services and technologies (10).
The combination of the extrinsic and intrinsic imperative for the inclusion of sustainability concerns implies a twofold mandate for health care that is maybe most clearly expressed in the notion of sustainable healthcare: Firstly, to advocate and contribute to improving sustainability at the general level of society in light of corresponding health implications and, secondly, ensure socially equitable healthcare services over time, where both are guided by the environmental constraints provided by our planetary ecosystem (11).
Positioning environmental sustainability in physiotherapy
A brief look at the notion of sustainability is needed to understand how the twofold sustainability mandate might be operationalised in physiotherapy. The predominant conception of sustainability (qua sustainable development) situates it as a middle ground or balancing of economic growth, social equity and environmental sustainability (12). This conception is likely to continue to receive much political support given its embeddedness in the SDGs as the largest corresponding multinational policy effort. However, this notion of sustainability has also been subject to in-depth critique alongside the development of alternative approaches, with pitfalls and arguments against it already pointed out well over two decades ago (13). One of the key criticisms of sustainability is related to its steadfast promotion of the colonial and capitalist model of development-through-economic-growth via policies like the SDGs (14,15). This criticism is raised because especially economic growth, carbon-fuelled industrialism and ongoing associated colonial practices are also the major causes of today’s environmental crisis, social exploitation and resulting health emergency (16).
Given the centrality of economic growth to the predominant conception of sustainability, it is not surprising that discourse in sustainable healthcare often risks advancing resonant approaches in which social equity, economic growth and environmental sustainability appear of equal importance (11,17,18). As long as this is the case, however, we should be concerned about the high likelihood that economic interests (for growth-as-sustainability) continue to override social questions of health, equity, and fundamental environmental needs for human health and flourishing.
To avoid perpetuating the same values, interests and practices that are driving today’s social, environmental and health crisis, we therefore propose considering a basic, but firm moderation from the very beginning of the physiotherapy profession’s engagement with sustainability. This moderation is already expressed in sustainable healthcare and increasingly influencing the sustainable development discourse, but it is emphasised more clearly in the field of planetary health, the research surrounding planetary boundaries and alternative economic ideas like Doughnut economy and
degrowth (1,19,20). Specifically, it is to ground our striving toward sustainability in the understanding that human health, societies, and economies depend on a planetary ecosystem that enables and supports them, and so position environmental sustainability as a fundamental endeavour (21).
Measuring environmental footprints
To take a first step in advancing environmental sustainability as a central concern in physiotherapy, in-line with the medico-ethical imperative of not doing harm, we suggest that measuring the environmental footprint of physiotherapy interventions should become a regular element of physiotherapy intervention research. In this article, we only point to a few basic terms and elements of environmental footprint measurement to consider potential benefits for practice and draw out some caveats, critical concerns and future questions.
A carbon footprint is understood as ‘the sum of greenhouse gas (GHG) emissions (which drive climate change) attributable to a given process’ (17). Elements such as infrastructure, energy, travel, tools and their production related to a service or product are converted into kilograms of carbon dioxide equivalents (CO2e) using GHG ‘emissions factors’ leading to a calculation of ‘carbon footprint (kg CO2e) = activity or resource use × GHG emissions factors’ (17). Carbon footprint calculation is continuously refining and more healthcare-specific guidance, including courses on measuring carbon-footprints in healthcare, as well as guidance on how to reduce carbon footprints can increasingly be found[1]. This provides a wide resource-base that could be drawn on and adapted to future physiotherapy intervention research.
In addition to measuring carbon-footprints, the wider environmental impact of physiotherapy interventions should also be considered. It has been noted that, in addition to GHG emissions, the overall environmental footprint of healthcare systems and services also includes extensive amounts of waste and air pollution, as well as the use of significant amounts of natural resources for transport and the development of specialist technologies (10,22). Calculation of the environmental impacts of these aspects is less common in healthcare so far, yet non-existent in physiotherapy to date. Jones (2009) already suggested that physiotherapists consider their carbon footprint and the environmental footprint of products used in practice well over a decade ago (23). Now, with only a decade left to achieve the goals set out in the UN Agenda 2030 and this year marking the beginning of the UN Decade on Ecosystems Restoration (https://www.decadeonrestoration.org/), we believe it is high time we followed this call and began measuring the broader environmental footprint of physiotherapy practiceto support the transition to more sustainable futures and ensure the health of present and future generations.
Clinical implications and caveats
One clinical implication of including the measurement of environmental footprints into physiotherapy intervention research will be the possibility to add a new, environmental layer to clinical reasoning in physiotherapy. If improving the environmental sustainability of all aspects of healthcare services is now a paramount requirement for healthcare professionals, then being able to make informed decisions based on relevant evidence of the environmental impact of physiotherapy services and in partnership with patients will be critical.
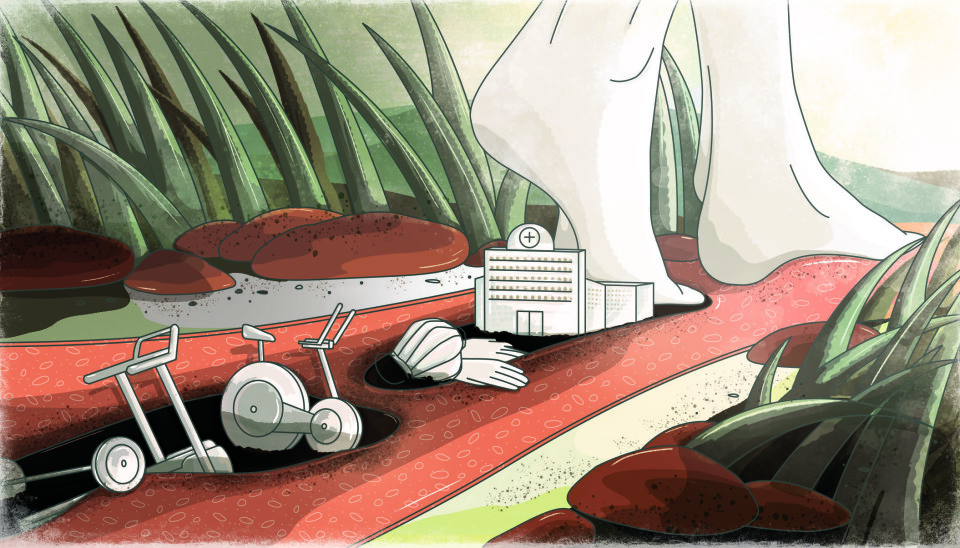
To take one example, environmental reasoning might become relevant to further the use of physiotherapy interventions over other modalities in the treatment of shoulder problems like subacromial pain syndrome or rotator cuff tears. Here, exercise-based interventions are both as effective as surgeries and significantly reduce the need for surgeries for these conditions (24). Surgeries in turn, have been identified to have a significant environmental footprint that adds to the even greater environmental cost of acute care and hospital stays in general (25). In contrast, there is growing evidence that physiotherapy – grounded in low-carbon interventions like movement, touch and communication – can reduce the need for hospital stays, as well as their length (26,27). More specific research is needed, however, to establish the comparative environmental footprint of physiotherapy and clarify if physiotherapy is not only equally effective clinically, but also more effective environmentally (i.e., more environmentally sustainable). If this is the case, health care systems, physiotherapists and patients could factor in broader and longer-term personal, and public health concerns relating to environmental sustainability into their decisions regarding personal health issues and rehabilitation pathways.
Along similar lines, more informed choices could also be made regarding gym-based exercise interventions as we consider their therapeutic and environmental effect compared to outdoors, or nature-based exercise interventions. Research in the latter field is growing exponentially and showing promising potential related to mental and physical health (28). Considering the natural resources required for the production of gym-equipment and the overall energy consumption of gym-equipment and spaces, there might be reason to believe that nature-based interventions could be a favourable alternative in some cases. The task for future research is to compare the therapeutic and environmental effects of these options against each other and provide indication as to which patients might benefit from nature-based interventions, and under what circumstances.
A similar situation might present itself, with regard to the rapid increase in physiotherapists engaging with and promoting telehealth and further digitalisation throughout the ongoing COVID-19 pandemic (29). Though it is often readily assumed that the transition to digital services has environmental benefits, this is not well established through research. Yet again, this makes evident the need for corresponding research to support clinical decision-making with the potential to improve patient health while also reducing environmental harm.
In terms of caveats, it should be emphasised that any recommendation of one intervention over another on the basis of additional environmental benefits must be as context specific as any other clinical recommendation. The particular environment, health needs, and lifeworld of each individual patient must be acknowledged in the clinical reasoning and decision-making process to identify the greater value of more environmentally sustainable options at the individual patient level. Scaling up to a broader, population health level, a difficult question that might arise is whether environmental concerns (with their population health implications) can override the health needs of individual patients, or not (e.g. where a patient needs resource intensive interventions and viable alternatives with a lower environmental footprint are missing or undesirable for individual reasons).
A further element that needs to be developed as we make progress in our efforts toward sustainability is the measurement of what we might refer to as the social footprint of healthcare. Staying close to questions of environmental sustainability in the present article, this might, e.g., pertain to questions about who produces the tools used in health care research and interventions, and under what conditions. Though approaches to measuring such social costs are far less developed than those for carbon- and environmental footprints (30), they must be considered if we are to achieve sustainable healthcare in a sense that does justice to the broader aspirations expressed in the notion of sustainability and the UN Agenda 2030 Sustainable Development Goals.
Conclusion
In this article we have made a first attempt at introducing environmental sustainability into clinical decision-making via the measurement of environmental footprints of physiotherapy interventions. Though much remains to be explored and adapted as physiotherapists make first advances in this urgent new field, measuring the environmental footprint of physiotherapy interventions is an essential first step toward the twofold mandate of sustainable healthcare: to improve the sustainability of health care systems and services, and contribute to the broader societal transition to sustainable futures. Evidence of environmental footprints of physiotherapy services has direct implications for physiotherapy clinical decision-making, but also health care systems more broadly speaking, as physiotherapy might prove itself the sustainable choice for a wide variety of health problems.
References
1) Steffen W, Richardson K, Rockstrom J, Cornell SE, Fetzer I, Bennett EM, Sorlin S. Planetary boundaries: Guiding human development on a changing planet. Science, 2015;347(6223):1259855. doi:10.1126/science.1259855
2) Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. The Lancet. 2021;397(10269):129-170. doi:10.1016/s0140-6736(20)32290-x
3) United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. Department of Economic and Social Affairs [Internet]. Sdgs.un.org. 2015 [cited 13 January 2021]. Available from: https://sdgs.un.org/2030agenda.
4) Barna S, Maric F, Simons J, Kumar S, Blankestijn PJ. Education for the Anthropocene: Planetary health, sustainable health care, and the health workforce. Medical Teacher. 2020;40(10):1091-1096. doi:10.1080/0142159x.2020.1798914
5) Maric F, Nicholls D. Paradigm shifts are hard to come by: looking ahead of COVID-19 with the social and environmental determinants of health and the UN SDGs. European Journal of Physiotherapy. 2020;22(6):379-381. doi:10.1080/21679169.2020.1826577
6) Elvén M, Hochwälder J, Dean E, Söderlund A. Predictors of Clinical Reasoning Using the Reasoning 4 Change Instrument With Physical Therapist Students. Physical Therapy. 2019;99(8):964-976. doi:10.1093/ptj/pzz044
7) Jones MA, Jensen G, Edwards I. Clinical reasoning in physiotherapy. Clinical reasoning in the health professions. 2008:245-56.
8) Higgs J, Jensen G, Loftus S, Christensen N. Clinical reasoning in the health professions. 3rd ed. Butterworth-Heinemann.
9) Karliner J, Slotterback S, Boyd R, Ashby B, Steele K, Wang J. Health care’s climate footprint: the health sector contribution and opportunities for action. European Journal of Public Health. 2020;30(Supplement_5).
10) Lenzen M, Malik A, Li M, Fry J, Weisz H, Pichler P et al. The environmental footprint of health care: a global assessment. The Lancet Planetary Health. 2020;4(7):e271-e279. doi: 10.1016/S2542-5196(20)30121-2
11) Mortimer F, Isherwood J, Wilkinson A, Vaux E. Sustainability in quality improvement: redefining value. Future Healthcare Journal. 2018;5(2):88-93. doi:10.7861/futurehosp.5-2-88
12) Brundtland G. Our common future: Report of the World Commission on Environment and Development. International Affairs. 1987;64(1):126-126.
13) Willers B. Sustainable Development: A New World Deception. Conservation Biology. 1994;8(4):1146-1148.
14) Kopnina H. Education for the future? Critical evaluation of education for sustainable development goals. The Journal of Environmental Education. 2020;51(4):280-291. doi: 10.1080/00958964.2019.1710444
15) Weber H. Politics of ‘Leaving No One Behind’: Contesting the 2030 Sustainable Development Goals Agenda. Globalizations. 2017;14(3): 399-414. doi: 10.1080/14747731.2016.1275404
16) Steinberger J, Lamb W, Sakai M. Your money or your life? The carbon-development paradox. Environmental Research Letters. 2020;15(4):044016. doi:10.1088/1748-9326/ab7461
17) Mortimer F, Isherwood J, Pearce M, Kenward C, Vaux E. Sustainability in quality improvement: measuring impact. Future Healthcare Journal. 2018;5(2):94-97. doi: 10.7861/futurehosp.5-2-94
18) Heggen K, Sandset T, Engebretsen E. COVID-19 and sustainable development goals. Bulletin of the World Health Organization. 2020;98(10):646-646. doi:10.2471/BLT.20.263533
19) Hickel J. What does degrowth mean? A few points of clarification. Globalizations. 2020;1-7. doi:10.1080/14747731.2020.1812222
20) Raworth K. A Doughnut for the Anthropocene: humanity's compass in the 21st century. The Lancet Planetary Health. 2017;1(2):e48-e49. doi:10.1016/S2542-5196(17)30028-1
21) Myers S, Frumkin H. Planetary Health: Protecting Nature to Protect Ourselves: Protecting Nature to Protect Ourselves. Washington, DC: Island Press; 2020.
22) NHS England [Internet]. Delivering a ‘Net Zero’ National Health Service. England.nhs.uk. 2021 [cited 13 January 2021]. Available from: https://www.england.nhs.uk/.
23) Jones L. Physiotherapy and the Earth's global climate: a need for cultural change. Physiotherapy Research International. 2009;14(2):73-76. doi:10.1002/pri.441
24) Kukkonen J, Joukainen A, Lehtinen J, Mattila K, Tuominen E, Kauko T et al. Treatment of non-traumatic rotator cuff tears. The Bone & Joint Journal. 2014;96-B(1):75-81. doi: 10.1302/0301-620X.96B1.32168
25) MacNeill A, Lillywhite R, Brown C. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. The Lancet Planetary Health. 2017;1(9):e381-e388. doi:10.1016/S2542-5196(17)30162-6
26) Pouwels S, Hageman D, Gommans L, Willigendael E, Nienhuijs S, Scheltinga M et al. Preoperative exercise therapy in surgical care: a scoping review. Journal of Clinical Anesthesia. 2016;33:476-490. doi:10.1016/j.jclinane.2016.06.032
27) Sobrinho MT, Guirado GN, Silva MA. Preoperative therapy restores ventilatory parameters and reduces length of stay in patients undergoing myocardial revascularization. Revista Brasileira de Cirurgia Cardiovascular. 2014;29(2). doi:10.5935/1678-9741-20140021
28) Stanhope J, Breed M, Weinstein P. Exposure to greenspaces could reduce the high global burden of pain. Environmental Research. 2020;187:109641. doi:10.1016/j.envres.2020.109641
29) Nicholls D, Groven KS, Røe Y, Dahl-Michelsen T, Bjørbækmø W. Is COVID showing us the future for physiotherapy? [Internet]. Fysioterapeuten.no. 2021 [cited 13 January 2021]. Available from: https://fysioterapeuten.no/covid-19-fagessay/is-covid-showing-us-the-future-for-physiotherapy/121849.
30) Leach M, Reyers B, Bai X, Brondizio E, Cook C, Díaz S et al. Equity and sustainability in the Anthropocene: a social–ecological systems perspective on their intertwined futures. Global Sustainability. 2018;1. doi:10.1017/sus.2018.12
Footnote
[1]Exemplary list of carbon calculators and related resources:
- http://css.umich.edu/factsheets/carbon-footprint-factsheet
- https://www.footprintnetwork.org/
- World Business Council for Sustainable Development 2011 The Greenhouse Gas Protocol;
- https://klimakalkulatoren.no/: The official Norwegian climate calculator (not ready for public use yet); https://www.nature.org/en-us/get-involved/how-to-help/carbon-footprint-calculator/;
- PAS 2050 (2011). Specification for the assessment of the life cycle greenhouse gas emissions of goods and services. Produced by the UK Government.
- https://practicegreenhealth.org/tools-and-resources/guide-going-carbon-neutral;
- https://sustainablehealthcare.org.uk/courses/carbon-footprinting-healthcare
© Author(s) (or their employer(s)) 2021. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions (https://creativecommons.org/licenses/by-nc/4.0/). Published by Fysioterapeuten.
























