
Norwegian primary health care: Evaluation of a lifestyle intervention program
Vitenskapelig artikkel i Fysioterapeuten 11/2013.
Silje Stangeland Lie, MSc og fysioterapeut. Doktorgradsstipendiat i Helsevitenskap, Universitetet i Stavanger. silje.s.lie@uis.no.
Cecilie Hagland Sevild, Fysioterapeut og prosjektleder Stor og Sterk/Frisklivssentralen, Avdeling for fysio- og ergoterapi, Stavanger Kommune. cecilie.hagland.sevild@stavanger.kommune.no.
Leif Inge Tjelta, Dosent, Institutt for grunnskolelærerutdanning, idrett og spesialpedagogikk. Universitetet i Stavanger.
Sindre Mikal Dyrstad, PhD, Førsteamanuensis, Institutt for grunnskolelærerutdanning, idrett og spesialpedagogikk. Universitetet i Stavanger.
Denne vitenskapelige originalartikkelen er fagfellevurdert etter Tidsskriftet Fysioterapeutens retningslinjer. Akseptert 17.9.2013.
Studien er godkjent av REK. Ingen interessekonflikter oppgitt.
Abstract
Aims: The aim of this study was to evaluate the physiological effects of an outpatient lifestyle intervention program prescribed by Norwegian primary health care for inactive obese people. The program includes exercise and lifestyle modification education.
Methods: Inactive obese participants were randomly assigned to either an intervention group (n=18), which received six months of intensive training and health education followed by six months of follow-up once a week, or to a control group (n=17). At baseline, six months and 12 months the participants were tested for anthropometrics, VO2max, blood lipids and blood pressure.
Results: Compared to the control group the intervention group reduced waist circumference and fat mass, and increased VO2max by 4.1%, 6.5% and 9.9%, respectively. The difference between the two groups was significant (p<0.05) after six months, but not after 12 months.
Conclusions: This small-scale study shows that this multidisciplinary outpatient lifestyle intervention program had beneficial effects on reducing several obesity-related cardiovascular risk factors after six months. However, in the conclusion several adjustments to this and similar programs are suggested to further improve the participants’ outcome and reduce drop-out.
Keywords: Obese, waist circumference, weight loss, blood pressure, VO2max, outpatient, randomised controlled trial.
Norsk sammendrag:
Stor og Sterk - Evaluering av et livsstilsendringsprogram i primærhelsetjenesten
Mål: Målet med studien var å evaluere fysiologiske effekter av et poliklinisk livsstilsendringsprogram i primærhelsetjenesten rettet mot inaktive personer med fedme. Programmet bestod av trening og undervisning vedrørende livsstilsendring og mestring.
Metoder: Inaktive deltakere med fedme ble randomisert til enten en intervensjonsgruppe (n = 18), som fikk seks måneder med intensiv trening og undervisning etterfulgt av seks måneder med oppfølging en gang i uken, eller til en kontrollgruppe (n = 17). Ved baseline, etter seks og 12 måneder gjennomførte deltakerne tester og målinger av antropometri, VO2max, blodlipider og blodtrykk.
Resultater: Sammenlignet med kontrollgruppen hadde intervensjonsgruppen oppnådd reduksjon av midjemål og fettmasse, samt økt VO2max med henholdsvis 4,1%, 6,5% og 9,9%. Forskjellen mellom de to gruppene var signifikant (p <0,05) etter seks måneder, men ikke etter 12 måneder.
Konklusjon: Denne studien, med de begrensningene den har, viser at det tverrfaglige livsstilendringsprogrammet Stor og Sterk reduserte flere fedme-relaterte kardiovaskulære risikofaktorer etter seks måneder. Programforbedringer foreslås for å ytterligere forbedre deltakernes resultater på lengre sikt, samt redusere frafall.
Nøkkelord: overvekt, fedme, midjemål, vektreduksjon, blodtrykk, VO2max, poliklinisk, randomisert kontrollert studie.
Introduction
One in five adults in Norway are obese and the prevalence is increasing (1), which makes the need for improved prevention and treatment strategies critical. Lifestyle programs are multi-component interventions that focus on promoting a healthy lifestyle with dietary education, physical exercise and behavioural modification (2, 3), and can be an alternative to treatment with gastric bypass surgery (4). Two lifestyle intervention trials in Norway with inpatient programs have proven to produce positive outcomes (4, 5), but to our knowledge no research has been conducted on outpatient programs in Norwegian primary health care.
In one of the larger cities in Norway, physiotherapists, occupational therapists and public health advisors have started an interdisciplinary lifestyle intervention program to help inactive obese people change their lifestyle. These types of programs are currently being conducted in an increasing number of cities all over the country because of the political priority in the health sector to prevent and reduce obesity and inactivity in the population and the establishment of «Healthy living centres» (Frisklivssentraler) (6). Efficacy studies of these small-scale intervention programs are needed to ensure and improve their quality. This study is unique as the participants had the opportunity to live at home and continue working while participating. The aim of the study was to investigate changes in participants’ anthropometrics, maximal oxygen uptake, blood pressure and blood lipids during a one-year outpatient lifestyle intervention program used in Norwegian primary health care.
Methods
Participants and design
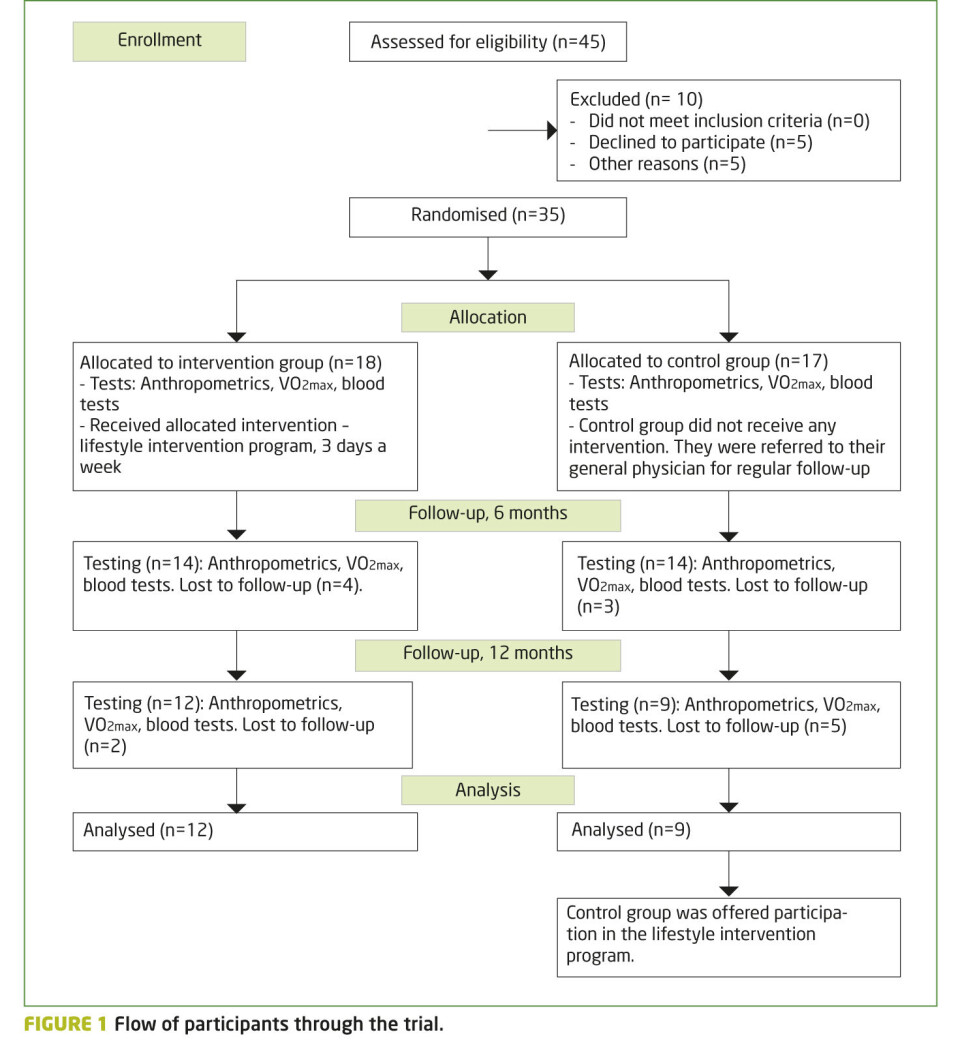
Participants were referred to the program by their own general physicians, and a total of 35 participants were included after meeting the inclusion criteria (age 18-65 years, BMI ≥ 35, inactive, independent in activities of daily living, living in the city where the intervention was executed). Exclusion criteria were severe psychiatric disorders and the inability to communicate in Norwegian. After obtaining informed consent from the participants, they were randomly assigned to either the intervention (n=18) or the control group (n=17). Dropouts are described in Figure 1 and table 5. The study was approved by the Regional Committee for Medical Research Ethics.
Figure 1
Procedures and tests
At baseline, six months and 12 months the participants underwent physical tests and measurements to investigate anthropometrics (waist circumference, body mass and body composition), blood pressure, blood lipids total-, HDL- and LDL cholesterol and triglycerides, and blood glucose level.
Primary outcome was to investigate whether the intervention group managed to obtain significantly greater improvements in waist circumference than the control group. Secondary outcomes of interest were body weight and composition, blood lipids, blood pressure and maximal oxygen uptake.
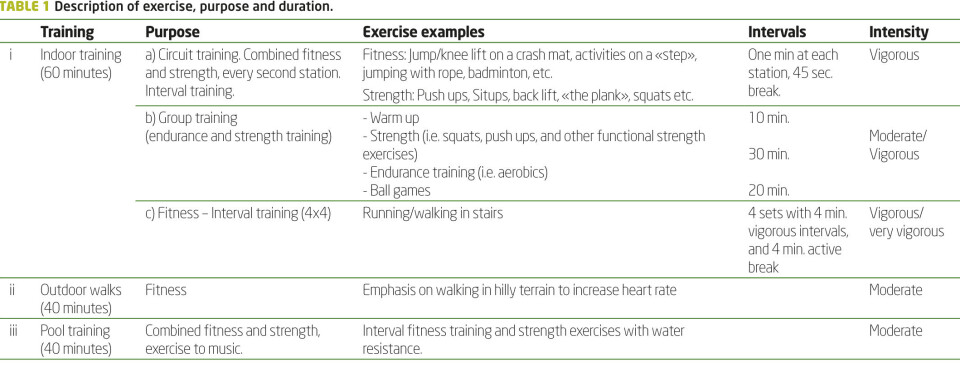
Table 1
Maximal oxygen uptake (VO2max) was tested by using a modified Balke protocol and with a Woodway treadmill1 as ergometer. Participants were connected to the oxygen measuring system, type Vmax 292, via a mask and a three-way directional valve3. The analyser was calibrated with room air and certified calibration gases. The participants started the test by walking at an incline of 4% at a speed of 3.8 or 4.8 km·h-1, depending on their physical fitness. After a four-minute warm up the incline was increased by 2% every minute until exhaustion. Heart rate was registered continuously during the test using a Polar Sport tester4. Blood lactate level was measured using Lactate Pro5. Borg’s Rating of Perceived Exertion was used to register participants’ exertion at the end of the test (7). Values of heart rate, blood lactate, Respiratory Quotient and perceived exertion of the three tests were compared to evaluate exhaustion level during the tests. These data are not presented since no participants were excluded due to large differences between these data. Blood pressure was tested in sitting position prior to the VO2max-test. Measurements were performed by a standard auscultatory method with an appropriate-sized cuff. The results are specified in mmHg. A calibrated digital scale6 was used to measure body weight. Waist circumference was measured in standing position from the point midway between the inferior margin of the last rib and the crest of the ileum. Body composition was analysed using InBody 720 analysis7. The participants had blood samples taken and analysed by their own general physician to measure blood lipids and blood glucose level. The participants were instructed by the project management to be fasting before blood sampling. Training attendance for each participant was recorded through the first six months.
Footnotes:
1) Woodway, ELG 2, Weil am Rhein, Germany, 2) Vmax 29, Medics Corporation, Yorba Linda, CA, USA 3) Hans Rudolf, Inc, Kansas City, USA 4) Polar Electro Oy, Kempele, Finland 5) LT-1710TM, KDK Corporation, Kyoto, Japan 6)Model 770, Seca Corp, Hamburg, Deutschland 7) BioSpace, Seoul, Korea
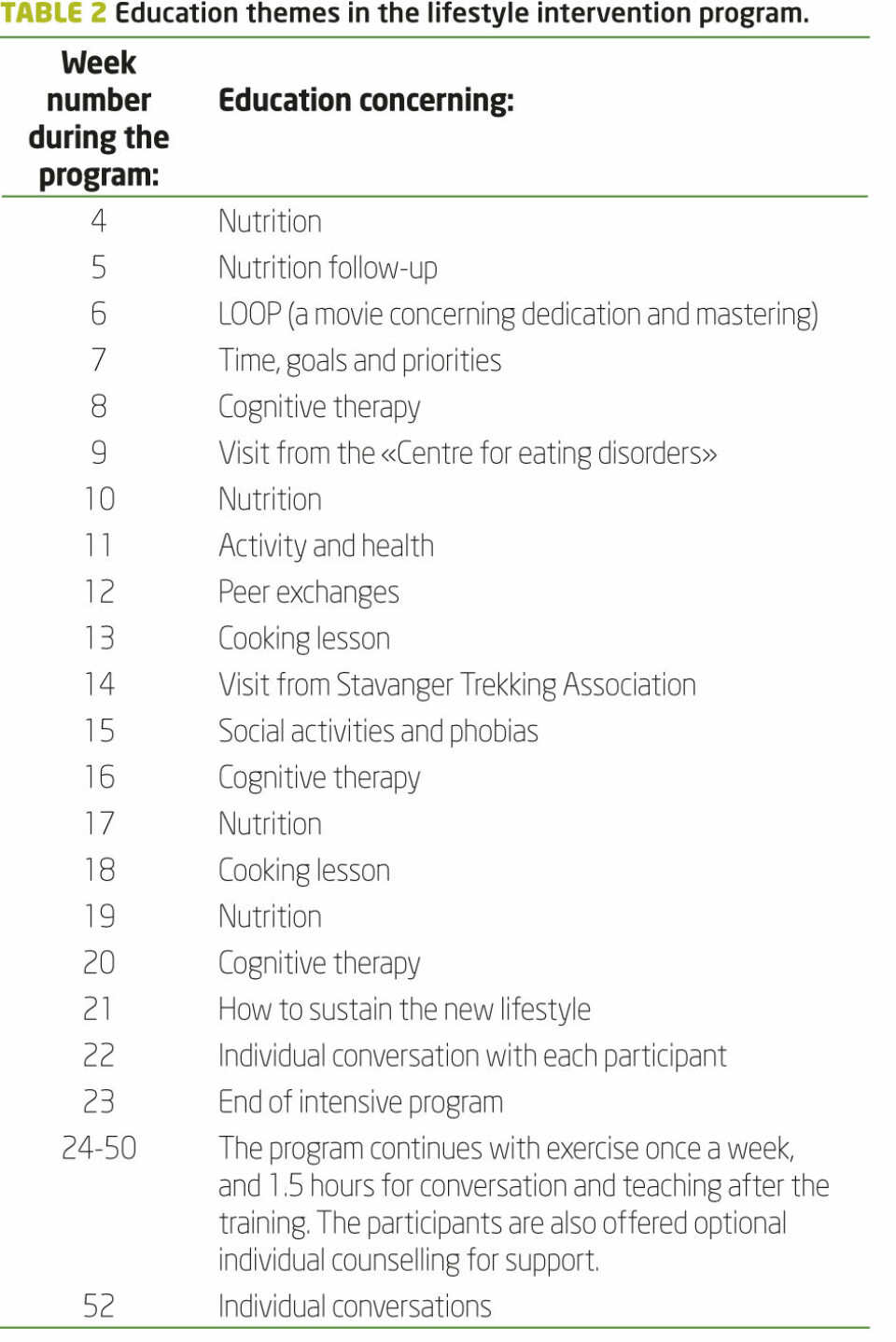
Table 2
Intervention
The treatment given to the participants in the intervention group for the first six months consisted of an organised group-based exercise program lasting 40-60 minutes, three days per week at daytime. This program consisted of three types of activities: i) indoor training including circuit training, strength training, high-intensity running, ball games and aerobics, ii) outdoor walks and iii) pool activities including endurance and strength training (table 1). The intensity level was moderate to vigorous.
Once a week prior to exercise, group education concerning different themes was given (table 2). The intervention group was also offered individual counselling with professionals trained in cognitive therapy. For the next six months they were offered organised physical exercise (40-60 minutes) and group education or conversations once a week, as well as individual counselling if requested.
Participants in the control group visited their general physician according to their own schedule, and were offered participation in the lifestyle intervention program after one year.
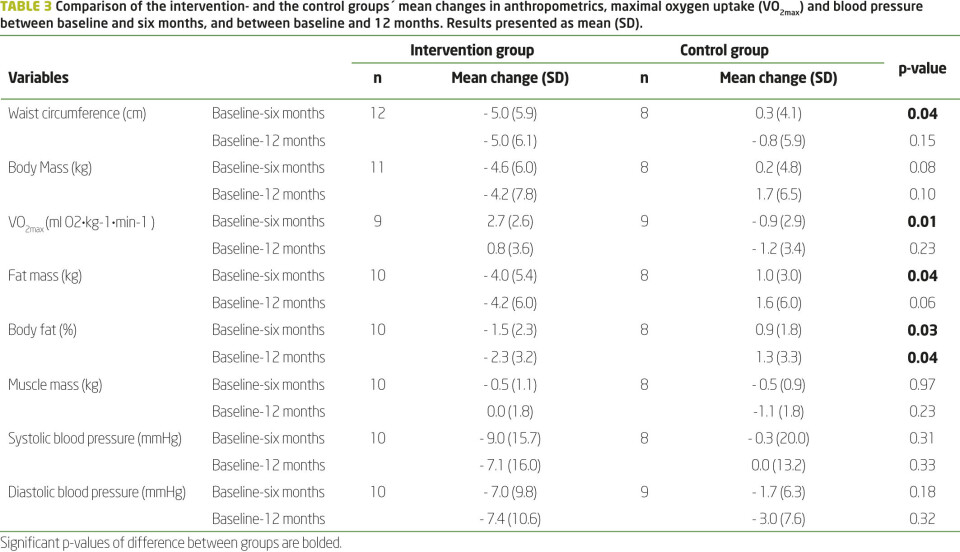
Table 3
Statistical analysis
Independent sample t-test was used to compare the mean changes between the intervention and the control groups´ baseline values with the values after six and 12 months respectively. In addition, a general line model for repeated measures was used to compare the physiological parameters within the control and intervention groups at baseline and follow up at six and 12 month (Table 4). Only participants who completed three tests are included. Because of the small sample and outliers the non-parametric Mann-Whitney U-test was executed on the parameters for controlling the results. Pearson’s product-moment correlation coefficient analysis was used to study the relationship between the change in physiological parameters (body weight, fat mass, waist circumference, VO2max) and exercise attendance. A probability value <0.05 was considered statistically significant. All statistical analyses were performed using IBM´s SPSS-18 for Mac for quantitative analysis. Data is expressed as mean (SD) unless otherwise specified.
Results
Comparison of mean changes in anthropometrics (waist circumference, body mass, body fat mass and muscle mass), as well as maximal oxygen uptake (VO2max) and blood pressure between the groups are shown in table 3.
During the first six months the intervention group reduced their waist circumference, fat mass and body mass by 4.1%, 6.5% and 3.7%, respectively. After 12 months these parameters had small mean changes, but larger SD. The control group had small to no change in these parameters, and the mean changes between the groups were significantly different after six months, but not after 12 months. The only exception was body fat in %, which decreased further in the intervention group after 12 months. VO2max increased in the intervention group by 2.7ml O2·kg-1·min-1 (9.9%) after six months, while the control group had a small decrease. After six months the difference in mean change between the groups was significant (p=0.01). After 12 months mean VO2max in the intervention group had decreased and was not significantly different from the baseline value. There was no significant difference in the mean change of VO2max from baseline to 12 months between the intervention and control group. The absolute VO2max in the intervention group increased from 2.92 to 3.04 l O2·min-1, or 4.1% the first six months while the control group’s corresponding values was reduced from 2.93 to 2.80 l O2·min-1, or -4.3%. This difference in absolute VO2max values was significant after 6 months (p= 0.03), but not after 12 months.
Table 4
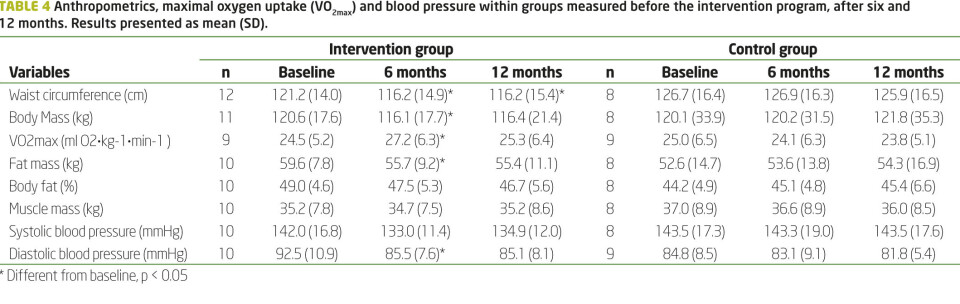
There was no significant difference in the mean change in diastolic and systolic blood pressure from baseline to six and 12 months between the intervention and control groups. The non-parametric test Mann-Whitney U-test confirmed the results from the parametric tests, and there was no difference in significance level between the parametric and non-parametric tests.
The mean changes in anthropometrics, maximal oxygen uptake and blood pressure within both groups are shown in table 4.
Although there was no significant difference in mean change of diastolic and systolic blood pressure between the groups, the intervention group showed a significant decrease of diastolic blood pressure; 7.6% after six months and 8% after 12 months (p<0.05). There were no significant changes for blood pressure in the control group.
With regard to the blood tests, there were no significant differences between the groups in mean changes when baseline values were compared to six and 12 months. In the intervention group there were no significant changes in the blood lipids total- and HDL cholesterol and triglycerides, as well as blood glucose. However, the level of LDL cholesterol increased by 12% from a mean of 3.07 (0.73) at baseline to a mean of 3.43 (0.75) after six months of intervention (p = 0.04). After 12 months it was no longer significantly higher than at baseline. There were no significant differences for the control group.
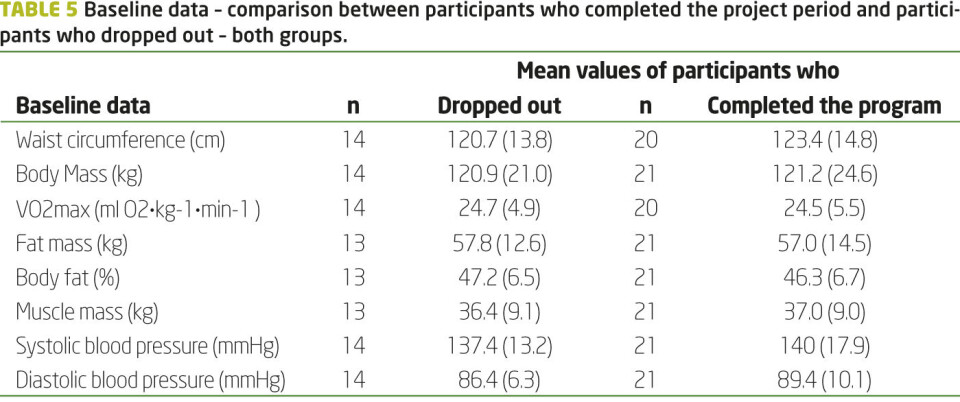
The participants in the intervention group attended on average 43 (14) of the 58 training sessions during the first six months of the lifestyle program (n= 14). After both six and 12 months, there were no significant correlations between the attended number of training sessions and the change in VO2max, body weight, fat mass and waist circumference. After six months the drop-out rate was 22% in the intervention group, and 18% in the control group. After 12 months the drop-out rate was 33% and 47%, respectively.
Baseline data on participants who dropped out compared to those who finished the program in both groups are presented in table 5. There were no significant differences between the former and the latter in these important health parameters at baseline.
Table 5
Discussion
The main findings of this study were that the intervention group compared to the control group experienced significantly greater reductions in waist circumference, body mass and body fat mass during the first six months of intervention. The participants also significantly increased their maximal oxygen uptake and lowered their diastolic blood pressure during this period. There were no further improvements during the next six months of the intervention, and the significant difference in mean changes between the groups was not maintained, except for body fat mass in %. The drop-out rate was high in both groups after 12 months, but higher in the control group.
Waist circumference is increasingly being looked upon as one of the more accurate tools of measurement of an individual’s risk for metabolic syndrome and cardiovascular disease (8, 9). The intervention group participants in this study reduced mean waist circumference by 5 cm. For the target group represented in this study, reducing waist circumference by 5 cm or more has health benefits and is described as a realistic target (10). The mean reduction of waist circumference was maintained after 12 months, even though the significant difference between the two groups and within the intervention group was not maintained because of increased standard deviation. This indicates that the program has a positive effect on this important health parameter for some of the participants.
Studies indicate that a gradual, modest weight reduction of 5-10% will reduce several obesity related cardiovascular risk factors, and greater weight loss can lead to increased improvements and maintenance (11, 12). The mean weight reduction in the intervention group was around 4%, during the first six months, with no further reduction seen at 12 months. The increase in VO2max of 9.9% in the intervention group was also limited to the first six months. This indicates that the intensive training period should be longer than six months, and the number of group training sessions should not have been reduced from three to one session during the last six months of the program. It seems that most participants in the intervention group did not manage to maintain the physical activity level needed to maintain the VO2max gained during the first six months of the intervention.
Even without weight loss, exercise makes a significant contribution to health benefits (13, 14). However, the present lifestyle program could focus more on diet and psychological reasons for overeating. Changing one’s diet seems to be one of the major challenges for participants in lifestyle intervention programs (5, 15). Burmeister et al. found that 19% of the overweight or obese people in their sample met criteria for food addiction (16). In this study, the intervention group received diet education, but it is possible that they did not manage to reduce their intake of saturated fats and carbohydrates because of food addiction. In terms of achieving weight loss, earlier research shows that physical activity alone is less effective than diet alone, and the combination of diet and physical activity has proven to have the greatest effect (17-19). The program in this study had a large focus on exercise, as the participants engaged in exercise three times a week for the first six months, totalling 58 training sessions. Diet education was offered six times, and cooking lessons were only offered two times during the six-month intensive project period. A recently published meta-analysis also states that diet and diet combined with exercise are superior to exercise only, for improving blood lipids in adults (20). None of the expected and desired changes in blood lipids were shown in the results from this study. The level of LDL cholesterol was increased in the intervention group after six months. Although this was unexpected, similar results were found by The Björknäs Study (15). The increase in LDL cholesterol may be explained by a diet high in saturated fats. Since some of the participants may have underlying eating disorders (16), they could benefit from more focus on diet education and cooking lessons, and psychological treatment for food addiction.
The European guidelines for classification of hypertension state that a blood pressure of 140/90 is regarded as mild hypertension, and a lower blood pressure is regarded as normal (21). Even though there was no significant difference in mean change of blood pressure between the two groups, the mean blood pressure in the intervention group improved during the intervention period, decreasing from mild hypertension (142/92; SD 16.8/10.9) to normal (135/85; SD 12.0/8.1). Of a total of 12 participants in the intervention group, seven had hypertension at baseline. Five out of the seven decreased their systolic blood pressure with at least 10 mmHg during the first six months of the program. The number of cardiovascular events has been found to decrease in step with the degree of blood pressure reduction (22), which indicates another positive effect the program has on an important health parameter.
Exercise attendance was registered for the intervention group, and participation varied greatly. However, we found no significant correlation between attendance at training and physical improvements. Some participants may not have trained intensively enough to achieve positive response from the exercise, indicating that some participants may need even closer follow-up and a more complementary program to achieve positive results. Other participants may have achieved positive results by their own efforts and by attending only parts of the program. This could indicate that some participants may benefit from attending only parts of the program, i.e. the measurements and some of the education, as they would be able to implement the needed lifestyle change with less follow-up. This points to the importance of individualised exercise programs and follow-up.
Earlier research indicates that regular follow-up and teaching of coping and behaviour modification strategies for this patient group is of great importance, if one is to achieve the lifestyle change with its desired effects (3). The control group visited their general physician according on their own schedule. This was insufficient for achieving weight loss and reducing cardiovascular risk factors in this study, as the control group showed no change in the parameters. This is also supported by previous research (23).
The drop-out rate was significant in both groups, but was higher in the control group. There were no important differences in baseline data between those who finished the program and those who dropped out (Table 5). In the intervention group the participants had peer exchanges, lessons and group exercise. The combination of these factors seems to be important in coping with a lifestyle change (3), which points to the importance of regular follow-up for this population. The reasons for dropping out or not completing all the tests varied, but seven out of 14 explained the drop-out with injury, illness or surgery. Compliance to treatment is a challenge in weight loss obesity treatment (24). Since this type of lifestyle intervention program is intensive, requires personal coaches and multiple sessions, a careful selection of motivated participants is needed to reduce drop-out rate and improve cost-effectiveness. It may be beneficial to develop a more individualised and differentiated approach in the future. Some participants could also preferably attend more comprehensive types of programs.
The main strengths of this study were the one-year intervention period and the extensive amount of data collected from each participant. We also collected useful experiences, which could be useful for similar intervention programs. However, the study has several limitations. First, because of limitations in the training facilities and limited finances of the municipality, only 18 patients could be included in the intervention program. The lack of control of the participants´ diet during the program is another limitation in the study-design. The diet could influence the participants´ ability to obtain the physiological changes we investigated in this study. There was also a large drop-out rate. Because this was a small-scale study, individual differences have a great impact on the mean results and standard deviation, thereby influencing the significance of the findings. Mean values could also be affected by outliers. However, data was re-analysed after exclusion of outliers, and these did not affect results of either the correlation tests or the compare means test. The results were also controlled by executing additional non-parametric statistics, with no change in significance levels.
Conclusion and implications for practice
This multidisciplinary outpatient lifestyle intervention program reduces obesity-related cardiovascular risk factors for the participants by improving participants’ anthropometrics, VO2max and blood pressure. The use of such programs in primary health care seems to be a good treatment for obese patients. However, based on experiences from this study, several adjustments in the program could be made to further improve the participants’ outcome. First, a careful selection of motivated participants seems important to reduce drop-out rate from the program. Second, it seems necessary to extend the intensive intervention program from six to 12 months. Third, individualised exercise programs are of great importance because of the participants´ varying motivation. A strategy for a broader and multidisciplinary follow-up of participants with complex problems is also needed. Fourth, to increase weight loss, participants need both more specialised help to change their diet, and an assessment for possible underlying eating disorders. Further research should evaluate the long-term effect that such programs have beyond the first year. It would also be of great interest to include surveys addressing the quality of life and self-perceived health changes in similar effect studies.
Acknowledgments
The study was funded by the Municipality of Stavanger and the University of Stavanger. No conflict of interest exists.
References
1. Helsedirektoratet. Forebygging, utredning og behandling av overvekt og fedme hos voksne. Nasjonale retningslinjer for primærhelsetjenesten. 2011. [cited 2013 19.06]; Available from: http://helsedirektoratet.no/publikasjoner/nasjonal-faglig-retningslinje-for-forebygging-utredning-og-behandling-av-overvekt-og-fedme-hos-voksne/Publikasjoner/nasjonal-faglig-retningslinje-for-forebygging-utredning-og-behandling-av-overvekt-og-fedme-hos-voksne.pdf
2. Galani C, Schneider H. Prevention and treatment of obesity with lifestyle interventions: review and meta-analysis. International Journal of Public Health. 2007;52:348-59.
3. Kirk SFL, Penney TL, McHugh T-LF, Sharma AM. Effective weight management practice: a review of the lifestyle intervention evidence. International journal of Obesity. 2012;36(2):178-85.
4. Hofsø D, Nordstrand N, Johnson LK, Karlsen TI, Hager H, Jenssen T, et al. Obesity related cardiovascular risk factors after weight loss: a clinical trial comparing gastric bypass and intensive lifestyle intervention. European Journal of Endocrinology. 2010;163 735-45.
5. Mæhlum S, Danielsen KK, Heggebø LK, Schiøll J. The Hjelp24 NIMI Ringerike obesity clinic: an inpatient programme to address morbid obesity in adults. British Journal of Sports Medicine. 2012;46:91-4.
6. Helsedirektoratet. Frisklivssentraler. 2011 [cited 2013 19.06]; Available from: http://helsedirektoratet.no/folkehelse/frisklivssentraler/Sider/default.aspx.
7. Borg G. Borg´s perceived exertion and pain scales. Champaign: Human Kinetics; 1998.
8. Knowles KM, Paiva LL, Sanchez SE, Revilla L, Lopez T, Yasuda MB, et al. Waist Circumference, Body Mass Index, and Other Measures of Adiposity in Predicting Cardiovascular Disease Risk Factors among Peruvian Adults. International journal of Hypertension. 2011;2011.
9. Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. American Journal of Clinical Nutrition. 2004;79:379-84.
10. Han TS, Richmond P, Avenell A, Lean ME. Waist circumference reduction and cardiovascular benefits during weight loss in women. International journal of Obesity Related Metabolic Disorders. 1997;21(2):127-34.
11. Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, et al. Benefits of Modest Weight Loss in Improving Cardiovascular Risk Factors in Overweight and Obese Individuals With Type 2 Diabetes. Diabetes Care. 2011;34(7):1481-6.
12. Barte JC, ter Bogt NC, Bogers RP, Teixeira PJ, Blissmer B, Mori TA, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obesity Reviews. 2010;11(12):899-906.
13. King NA, Hopkins M, Caudwell P, Stubbs RJ, Blundell JE. Beneficial effects of exercise: shifting the focus from body weight to other markers of health. British Journal of Sports Medicine. 2009;43:924-7.
14. Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. Medicine & Science in Sports & Exercise. 1999;31(11):646-62.
15. Eriksson KM, Westborg CJ, Eliasson MCE. A randomized trial of lifestyle intervention in primary healthcare for the modification of cardivascular risk factors. The Björknäs study. Scandinavian Journal of Public Health. 2006;34:453-61.
16. Burmeister JM, Hinman N, Koball A, Hoffmann DA, Carels RA. Food Addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite 2013;60:103-10.
17. Wing RR, Venditti E, Jakicic JM, Polley BA, Lang W. Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care 1998;21:350-9.
18. Wood PD, Stefanick ML, Dreon DM, al. e. Changes in plasma lipids and lipoproteins in overweight men during weight loss through dieting as compared with exercise. New England Journal of Medicine 1988;319:1173-9.
19. Hagan RD, Upton SJ, Wong L, Whittam J. The effects of aerobic conditioning and/or caloric restriction in overweight men and women. Medicine & Science in Sports & Exercise 1986;18:87-94.
20. Kelley GA, Kelley KS, Roberts S, Haskell W. Comparison of aerobic exercise, diet or both on lipids and lipoproteins in adults: A meta-analysis of randomized controlled trials. Clinical Nutrition. 2012;31:156-167.
21. Goran M, Fields DA, Hunter GR, Herd SL, Weinsier RL. Total body fat does not influence maximal aerobic capasity. International journal of Obesity Related Metabolic Disorders. 2000;24(7):841-8.
22. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Journal of Hypertension. 2007;25:1105-87.
23. Lindholm L, Ekblom T, Dash C, Eriksson M, Tibblin G, Schersten B. The impact of health care advice given in primary care on cardiovascular risk. British Medical Journal. 1995;310.
24. De Panfilis C, Cero S, Dall´Aglio E, Salvatore P, Torre M, Maggini C. Psychopathological predictors of compliance and outcome in weight-loss obesity treatment. Acta Bio Medica. 2007;78:22-8.

























