Changes in diet during a lifestyle intervention program for inactive obese
Vitenskapelig artikkel i Fysioterapeuten 6/2014.
Merete H. Helland, PhD, førsteamanuensis, Institutt for grunnskolelærerutdanning, idrett og spesialpedagogikk. Universitetet i Stavanger. merete.h.helland@uis.no
Sindre M. Dyrstad, PhD, førsteamanuensis, Institutt for grunnskolelærerutdanning, idrett og spesialpedagogikk. Universitetet i Stavanger
Denne vitenskapelige artikkelen er fagfellevurdert etter Fysioterapeutens retningslinjer, og akseptert 26.2.2014. Ingen interessekonflikter oppgitt.
Abstract
Aim: The primary aim of this study was to investigate changes in diet during a one year lifestyle intervention program, provided by Norwegian primary health care.
Design: A total number of 35 inactive and obese individuals participated in a randomized, controlled trial.
Methods: Food Frequency Questionnaire (FFQ) and Food Dairy (FD) were used to estimate dietary intake. At baseline, after six and 12 months participants filled out a four-day FD and at baseline and after 12 months FFQ was also included. The first six months consisted of physical training, organised as group-based exercise program lasting 40-60 minutes three days per week, and health education consisting of nutrition education, practical cooking and Cognitive Behavior Therapy (CBT), lasting 120 minutes for each component, every time. The last six months the participants were followed up once a week.
Results: No significant differences in total energy intake were found between the intervention- and control group. The intervention group decreased their body weight by 2.3%, while the control group increased their body weight by 3.5% (difference between groups, p = 0.081).
Conclusions: The intervention group did not show any significant changes in their diet, and found it more difficult to change their diet than to start exercise. To change the participants existing diet it is suggested to extend the intensive intervention period to 12 months and to increase focus on nutrition education, CBT and practical cooking.
Keywords: Food Diary; Food Frequency Questionnaire; obesity; intervention; body weight.
Tittel: Kostholdsendringer hos alvorlig overvektige deltakere i et livsstilsendringsprogram
Sammendrag
Hensikt: Målet med studien var å undersøke kostholdsendringer hos personer med fedme gjennom et ett-årig livsstilsendringsprogram igangsatt av primærhelsetjenesten.
Design: 35 inaktive, overvektige personer deltok i et randomisert, kontrollert forsøk.
Metoder: Matfrekvens (Food Frequency Questionnaire /FFQ) og kostdagbok (Food Dairy/FD) ble benyttet for å kartlegge kostholdet. En fire-dagers FD ble loggført ved oppstart, seks og 12 måneder. Ved baseline og 12 måneder ble også FFQ fylt ut. De første seks månedene besto av intensiv trening (tre gruppetreninger per uke, hver på 40-60 minutter), undervisning i ernæring og helse (fem leksjoner med ernæring, to ganger praktisk matlaging og fire leksjoner i kognitiv terapi, alle på 120 minutter hver) etterfulgt av ukentlig oppfølging i seks måneder.
Resultater: Det ble ikke funnet signifikante endringer i totalt energiinntak som følge av intervensjonen. Intervensjonsgruppen hadde en vektreduksjon på 2.3%, mens kontrollgruppen økte kroppsvekten med 3.5% (p for differansen mellom gruppene = 0.081).
Konklusjon: Deltakerne syntes det var vanskeligere å endre kostholdet enn å starte opp med trening. For å endre kostvaner bør intervensjonsperioden vare i minst ett år og større fokus bør rettes mot ernæring, kognitiv terapi og praktisk matlaging.
Nøkkelord: Kostdagbok; matfrekvensskjema; overvekt; intervensjon; kroppsvekt.
Introduction
According to estimates from World Health Organization, more than 1.4 billion adults are overweight (Body mass index (BMI) > 25 kg/m²) and of those, more than 200 million men and nearly 300 million women are obese (BMI > 30 kg/m²) (1).
The need for intervention programs for obese people within the Norwegian health care is increasing. The Norwegian Directorate of Health recommends that all Norwegian primary health care patients with BMI > 35 should be offered an individual evaluation and possible inclusion in an intervention program, as an alternative to bariatric surgery (2). Lifestyle interventions also give more favorable dietary 1-year changes than gastric bypass surgery in morbidly obese patients (3). To provide treatment for patients with an obesity problem, several municipalities in Norway are now starting lifestyle intervention programs. Lifestyle interventions can contribute to successful outcomes in different ways, whether it is diet alone, diet and exercise, exercise alone, meal replacements, very low energy diets, weight-loss medications or advice alone (4, 5, 6). A review of psychological pre-treatment predictors of weight control is given by Teixeira et al. (7). As far as we know, no research has been conducted on diet changes in outpatient programs in Norwegian primary health care. Effect studies of these small scale programs are rare, but highly important to improve their quality. In Stavanger, an outpatient lifestyle intervention program for obese people was established in 2009. New patients are enrolled in the program once or twice a year. The program is most comprehensive during the first six months, but patients are followed up during one year.
In this intervention program participants lived at home, together with their family, at the same time as participating in the intervention program. The main purpose of this study was to investigate changes in diet for inactive obese, during a 12-month lifestyle intervention program provided by Norwegian primary health care.
Methods
Study design
Thirty-five participants, all referred by their family doctor, were included in the study. Inclusion criteria were BMI ≥ 35 kg/m², living in the city of Stavanger and inactive but not depending on any technical resources. Exclusion criteria were severe psychiatric disorders and inability to communicate in Norwegian. They were randomly assigned to either a lifestyle intervention- or a control group. Data collection was carried out from September 2010 until September 2011. Study design is shown in table 1. Eighteen completed the Food Frequency Questionnaire (FFQ) at both baseline and after 12 months. When considering these 18 individuals, 15 also completed the Food Diary (FD) and the anthropometric analysis at baseline, six and 12 months, which explains the differences in n.
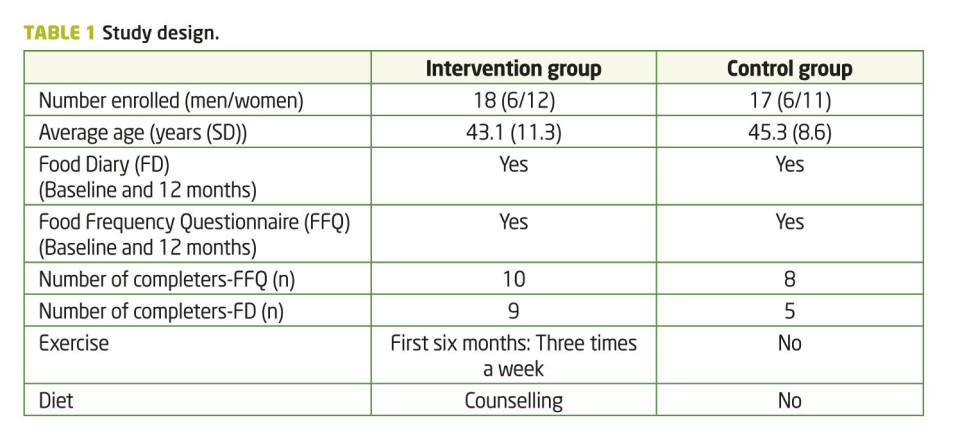
The treatment given to the participants in the intervention group consisted of an organized group-based exercise programme of 45-60 minutes (including changing), three days per week for the first six months. This programme consisted of three types of activities: i) gym activities including circuit training, strength training, high-intensity running, ball games and aerobics, ii) outdoor walks and iii) pool activities including endurance and strength training. Detailed information on the intervention is presented by Lie et al. (8). During the first 22 weeks, prior to exercise, participants were given nutrition education on five different occasions, two practical cooking lessons and four sessions with Cognitive Behavior Therapy (CBT; Table 2). All sessions lasted two hours each.
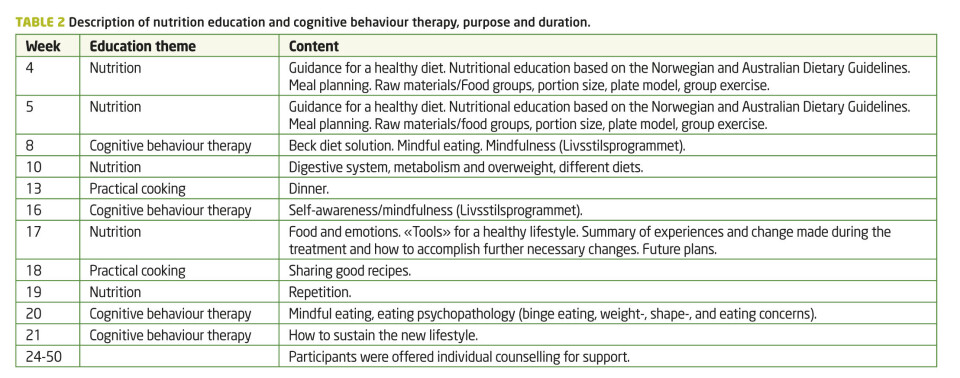
Nutritional advice was according to The Norwegian Directorate of Health (2). Recommendations related to Nutritional advice on portion size and meal planning was according to Dietary guidelines for Australians (9). Participants were not instructed to count calories, but requested to choose foods low in salt, to limit the intake of saturated fat, total fat and alcohol, and to consume only moderate amounts of sugar and food containing added sugar. In combination with dieting, CBT has been proven to benefit weight loss: how to think differently, change eating behavior, and lose weight permanently. The method used in this intervention study is based on the lifestyle program, «Livsstilsprogrammet», and is derived and translated to Norwegian from «The Beck Diet Solution» (10, 11).
During the intervention period, participants were offered additional individual counselling with a professional nutritionist, but at their own cost. The following six months they were offered organised physical exercise and group teaching or conversations once a week, as well as individual counselling if requested. The control group visited their general physician based on their own schedule, and were offered participation in the lifestyle intervention program after one year. The study was approved by the Regional Ethics Committee for Medical Research before subject recruitment and written informed consent was obtained from all subjects.
Food registration
Food Frequency Questionnaire (FFQ) is a validated tool for estimating dietary intake over a defined period of time, as opposed to specificity on a given day (12), while Food Diary (FD) gives an overview over energy consumed during selected days. Participants completed food records before entering the lifestyle change program and approximately six and 12 months later (Table 1). A four-day (three weekdays and one weekend day) weighed FD was completed. FFQ comprised about 270 questions and also included intake of dietary supplements, frequency and dose. The software program «Mat paa data» (13) and the Norwegian food composition table (14) were used for calculating amounts of nutrients and food reported. The FFQ was an extended and revised version of the semi-quantitative FFQ used in the Norwegian nationwide survey NORKOST 1997 (15). Average daily intake of energy and nutrients from the FFQ was computed/scanned using the food database KBS AE-07 and KBS software system (KBS, version 4.9, 2008) developed at the Department of Nutrition, University of Oslo, Norway. The food database KBS AE-07 is based on the 2006 edition of the Norwegian food composition table (13).
Anthropometric measurements
Body weight was measured using a calibrated, digital scale (Seca model 770, Seca GmbH & Co, Hamburg, Germany) with participants wearing light clothes and no shoes. Body height was measured to the nearest 0.5 cm using a stadiometer. Waist circumference (cm) was measured in standing position from the point midway between the inferior margin of the last rib and the crest of the ileum.
Statistics
To study differences between the control- and intervention group, an independent sample t-test was used. A paired sample test was used to measure differences between mean daily energy intake at baseline and after intervention in the two groups. Data are presented as means (standard deviation). Of the participants in the project, a p-value of less than 0.05 was regarded as statistically significant. A p-value between 0.05 and 0.1 indicated a tendency. Statistical analysis was performed using PASW Statistics 18 (SPSS Inc., Chicago, IL).
Results
At baseline, there were no significant differences in average energy consumption between drop-outs (11.6±1.7 MJ) and participants completing the intervention (11.4±5.1 MJ).
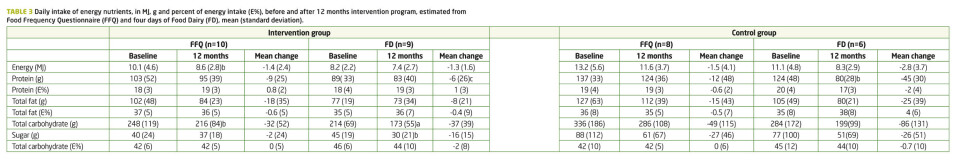
Results from the FD showed a reduction in protein intake by 6% and 35% in the intervention- and control group, respectively. Otherwise, no significant differences between the mean changes in energy nutrients were found between the intervention and control group at baseline and 12 months (Table 3), or between baseline and six months.
For individuals in the intervention group, a tendency of a 15% decrease in total energy intake was observed when comparing results from baseline and after 12 months and measured by FFQ (p = 0.099). The intervention group reported a 13% reduction in the consumption of total carbohydrates during the intervention period, indicating a tendency towards significant reduction (p = 0.082) when analyzing data from the FFQ. This observed reduction was supported by data from the FD, where this reduction was shown to be significant (-18%, p = 0.01). The consumption of added sugar in the intervention group was also reduced (-29%, p = 0.063) in data retained from the FD. Even though this reduction seems large, high standard deviations (SD) influence the significance level. Similar reductions as those shown for the intervention group were also found for the control group, although these results did not tend to be significant.
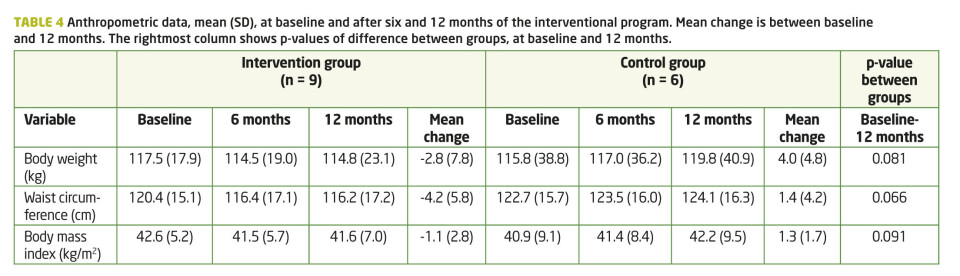
There were no significant differences in anthropometric data at baseline between the control- and intervention group. The change in body weight and waist circumference between baseline and 12 months tended to be different between the two groups for both body weight and waist circumference (Table 4). Although not significant, the intervention group decreased their body weight and waist circumference by 2.3% and 3.5%, respectively, while the control group increased their body weight by 3.5% and waist circumference by 3.2%.
Discussion
The main findings in this study were that only small, non-significant changes in the daily consumption of energy were detected in both the intervention- and control group during the 12-month intervention period.
Diet and energy intake
Participants found it difficult to make simultaneous changes related to both food intake and physical activity. They reported that it was easier to increase their physical activity level than to change their diet. Even though the control group increased mean body weight by 4.0 kg (3.5%), and the intervention group decreased body weight by 2.8 kg (2.3%) during 12 months, the changes were not significant and low compared to other studies, where favorable changes in both diet and weight circumference are reported, but most often the participants then eat a strict diet (16, 17). Maintaining weight loss has also been found to be positively related to self-monitoring, goal setting, social support, and length of treatment (18). Regain of body weight is associated with inconsistent and restrictive dieting, life stress, negative coping style, and emotional or binge eating patterns (19). Despite difficulties in reducing weight, lifestyle changes including increased physical activity and dietary changes will facilitate other beneficial health effects at a moderate weight loss, such as improved metabolic profiles, physical activity, self-esteem, body image, self-efficacy, quality of life, and functional capacity (20). However, several participants in the present study suffered from food addiction and depression, factors that might interfere with successful weight loss maintenance (21). Whether participants in this intervention program managed to change their diet varied, based on their intrinsic motivation and advice from clinical dietician, and the results show large standard deviations. Establishing an optimal meal pattern may be important in order to reduce the craving for high-carbohydrate snacks throughout the day.
There is a general prevalence in underreporting energy intake by using food registration (22, 23), and both FFQ and FD have challenges with underreporting, giving socially acceptable answers or changing eating habits during documentation (24). Body size influences the underreporting of energy intake and measuring nutrient intake has been shown to be more difficult among younger women (30-50 years) and overweight men and women (BMI >25 kg/m2) than among others (12, 25). FFQ might be more accurate for groups than for individuals, when considering misreporting of food items or difficulties in reporting correct portion size (26). At the same time it is a quick, easy, self-administered and inexpensive form of diet history. Although not significant, results reported with FD were lower than results reported with FFQ. When reporting diet for four days it is easy to change eating pattern or to eat less than normal. Some of the participants also reported eating disturbances, including periods with cravings for high fat food, followed by periods compensating with an extremely healthy eating pattern. Few of the participants owned a digital weight, which might also increase the possibility of underreporting. Despite the statistical limitations with FFQ, this is an acceptable method as guidance in interventions with economic restraints. Using FD is time consuming, expensive and probably also lead to underreporting. A 24-hour recall might be an alternative, but is more vulnerable for daily changes. However, underreporting did not seem to distort the main conclusion of these dietary surveys since the mean changes for most energy nutrients, reported from both methods, were not significantly different.
The only significant difference found between the intervention- and control group was a larger reduction in protein consumption in the control group, measured with FD (p=0.03). However, both the control- and intervention group consumed protein according to recommended daily intake (between 10 and 20% of energy intake). No other differences in diet were found after the intervention period, which indicate the need for more focus on motivation and/or diet among future participants. However, during 12 months the intervention group reduced their carbohydrate consumption by 13%, which may have led to the 15% reduction in total energy consumption detected with the FFQ (p < 0.099). Nutritional advice during the intervention focused on dietary patterns to promote health and well-being rather than recommending what to eat, or completely avoid. Participants were requested to reduce consumption of sugar and food containing added sugar. Emphasizing the importance of a regular meal plan might have reduced the amount of snacking, with the observed reduction in carbohydrates. Although not significant, the control group also reduced their energy intake by 12% (FFQ) and 25% (FD) during the project year, probably because of a higher focus on diet and exercise by participating in the project. High self-efficacy towards eating behaviors has been proposed as perhaps the only predictor of subsequent weight loss (27). Cognitive behavioral treatment programs have been developed as a tool to encourage health care professionals to become more active in preventing and treating obesity in the long term (28).
Suggested program changes
None of the participants paid for an individual diet counselling session. Since participants needed help to decide what to change and how to change their diet, individual diet counselling focusing on very specific goals and self-control should be included in the intervention (18, 29).
Participants in the intervention group were offered three training sessions a week, totalling 58, during the first six months of the lifestyle program. During the same period, five sessions with nutrition education, four sessions with CBT and two practical cooking lessons were offered. Underestimating the effect of nutritional education, CBT and practical cooking might have caused the observed lack of significant results regarding both diet and anthropometric measurements. A larger focus should be on diet (individualized nutritional counseling), practical cooking, and how to choose ingredients in their local store.
Limitations of the study
Even if all participants in the intervention group were included, the largest limitations of this study are the small number of participants (n= 37) and the large number of drop-outs (n= 17 or 46%). The number of participants in this study was limited by resources available in the municipality of Stavanger. The large drop-out numbers were caused by injuries, illness, low motivation to filling out the FFQ/FD questionnaires and low adherence to the program. Exclusion of this many participants may increase the possibility that the non-significant changes in diet and body-weight could be influenced of both type I and type II-error. The small sample size is also an important reason for the large SD found for all variables. Although a few significant results were found in the intervention group, this may have been caused by the larger sample size in the intervention group, compared with the control group. However, since no published data from such a Norwegian outpatient program exists, the trends found in the present study could be of great interest to improve the quality of future interventions for this patient group.
Conclusions
No significant difference was found between the intervention- and control group regarding total intake of calories. Even though the control group increased mean body weight and the intervention group decreased body weight, the changes were small. Future interventions should therefore include more guidance in changing participants’ diet. It seems to be important to normalize eating patterns, emphasize exercise, to set realistic goals regarding both weight and physical activity and to ensure social support through-out the intervention period.
Acknowledgments
The study was funded by the Municipality of Stavanger and the University of Stavanger. No conflict of interest exists.
References
1. WHO. Obesity and overweight 2012 [Fact sheet N°311]. http://www.who.int/mediacentre/factsheets/fs311/en/ [cited 10.01.14].
2. The Norwegian Directorate of Health. National Guidance for prevention, exposition and treatment of overweight and obesity among adults. Contract No.: IS-1735. 2011 (in Norwegian).
3. Johnson LK, Andersen LF, Hofsø D, Aasheim ET, Holven KB, Sandbu R, et al. Dietary changes in obese patients undergoing gastric bypass or lifestyle intervention: a clinical trial. The British Journal of Nutrition. 2013;110(1):127-34.
4. Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-Loss Outcomes: A Systematic Review and Meta-Analysis of Weight-Loss Clinical Trials with a Minimum 1-Year Follow-Up. Journal of the American Dietetic Association. 2007;107(10):1755-67.
5. Kirk S, Penney T, McHugh T-L, Sharma A. Effective weight management practice: a review of the lifestyle intervention evidence. International Journal of Obesity. 2012;36:178-85.
6. Galani C, Schneider H. Prevention and treatment of obesity with lifestyle interventions:review and meta-analysis. International Journal of Public Health. 2007;52:348-59.
7. Teixeira PJ, Going SB, Sardinha LB, Lohman TG. A review of psychosocial pre-treatment predictors of weight control. Obesity Reviews. 2005;6(1):43-65.
8. Lie Stangeland S, Sevild Hagland C, Tjelta LI, Dyrstad SM. Norwegian primary health care:Evaluation of a lifestyle intervention program. Fysioterapeuten. 2013(11):16-22.
9. Australian Government. Food for health- Dietary guidelines for Australians. Department of Health and Ageing. 2005. p. 28. (http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/n31.pdf).
10. Beck J. The Beck Diet Solution: Train Your Brain to Think Like a Thin Person. Reprint edition (February 3, 2009) ed. USA: Oxmoor House, Inc.; 2009. 288 p.
11. Johansen V, Andreassen R. Livsstilsendring og vektredusjon med kognitiv terapi og oppmerksomhetstrening. Tidsskrift for kognitiv terapi. 2010;11(4):7-14.
12. Andersen LF, Tomten H, Haggarty P, Lovo A, Hustvedt BE. Validation of energy intake estimated from a food frequency questionnaire: a doubly labelled water study. European Journal of Clinical Nutrition. 2003;57(2):279-84.
13. Mat paa data 2006. http://www.norwegianfoodcomp.no/# [cited 15.01.2014]
14. Rimestad AH, Borgejordet, Å, Vesterhus, KN, Sygnestveit, K, Løken, EB, Trygg, K, Pollestad, ML, Lund-Larden, K, Omholt-Jensen, G, Nordbotten, A. Statens råd for ernæring og fysisk aktivitet, Statens næringsmiddeltilsyn og Institutt for ernæringsforskning, Universitet i Oslo. Oslo: 2001.
15. Andersen LF, Nes M, Lillegaard IT, Sandstad B, Bjorneboe GEA, Drevon CA. Evaluation of a quantitative Food Frequency Questionnaire used in a group of Norwegian sdolescents. European Journal of Clinical Nutrition. 1995;49(8):543-54.
16. Robertson L. Lifestyle change intervention in a group of morbidly obese persons: effects on dietary habits, weight, waist circumference, and levels of adiponectin and C-reactive protein. Master thesis Bergen: The University of Bergen, 2007.
17. Collins CE. Dietary Strategies for Successful Weight Loss and Maintenance: More Evidence Required. Journal of the American Dietetic Association. 2011;111(12):1822-5.
18. Foster GD, Makris AP, Bailer BA. Behavioral treatment of obesity. The American Journal of Clinical Nutrition. 2005;82(1):230S-5S.
19. Foreyt JP, Goodrick GK. Attributes of successful approaches to weight loss and control. Applied and Preventive Psychology. 1994;3(4):209-15.
20. Aadland E, Anderssen SA. Treadmill Calibration of the Actigraph GT1M in Young-to-Middle-Aged Obese-to-Severely Obese Subjects. Journal of Obesity. 2012;2012:1-8.
21. Wing RR, Phelan S. Long-term weight loss maintenance. The American Journal of Clinical Nutrition. 2005;82(1 Suppl):222S-5S.
22. Birgisdottir B, Kiely M, Martinez J, Thorsdottir I. Validity of food frequency questionnaire to assess intake of seafood in adults in three European countries. Food control. 2008(19):648-653.
23. Scagliusi FB, Ferriolli E, Pfrimer K, Laureano C, Cunha CS, Gualano B, et al. Underreporting of Energy Intake in Brazilian Women Varies According to Dietary Assessment: A Cross-Sectional Study Using Doubly Labeled Water. Journal of the American Dietetic Association. 2008;108(12):2031-40.
24. Tucker KL. Assessment of usual dietary intake in population studies of gene-diet interaction. Nutrition Metabolism and Cardiovascular Diseases. 2007;17(2):74-81.
25. Paalanen L, Männistö S, Virtanen MJ, Knekt P, Räsänen L, Montonen J, et al. Validity of a food frequency questionnaire varied by age and body mass index. Journal of Clinical Epidemiology. 2006;59(9):994-1001.
26. Brown D. Do Food Frequency Questionnaires Have Too Many Limitations? Journal of the American Dietetic Association. 2006;106(10):1541-3.
27. U.S.DHHS, NIH-National Heart, Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. NIH Publication No. 98-4083, 1998.
28. Melin I, Rössner S. Practical clinical behavioral treatment of obesity. Patient Education and Counseling. 2003;49(1):75-83.
29. Haws KL, Redden JP. In control of variety. High self-control reduces the effect of variety on food consumption. Appetite. 2013;69:196-203.

























