
Subacromial impingement syndrome and rotator cuff tendinopathy: The dilemma of diagnosis.
Fagkronikk i Fysioterapeuten 9/13
Dr Jeremy S Lewis PhD MSc (Manipulative Physiotherapy) FCSP. Consultant Physiotherapist, Sonographer. Research and Innovation Lead, Health at Stowe, Central London Community Healthcare NHS Trust. Reader in Physiotherapy Research, University of Hertfordshire, Hertfordshire, UK. Email: jeremy.lewis@LondonShoulderClinic.com. Web: www.LondonShoulderClinic.com
This chronicle was accepted on March 6th, 2013. Chronicles are not peer reviewed. Epublish Ahead of Print (23.4.13).
Introduction
Musculoskeletal pathology involving the shoulder is associated with substantial morbidity and loss of function that increases with age (1-3). It is generally considered that effective treatment is dependent upon understanding the mechanism of onset together with identification of the structure(s) involved with the symptoms and excluding those not involved. Mechanisms may involve; trauma, inappropriate ergonomic set-up, posture, repetitive and / or unaccustomed loading, systemic illness, local disease, or be idiopathic. Following routine clinical procedures that include; observation, assessment of active and passive movements, palpation, and resistance tests, a series of orthopaedic tests are commonly applied to identify the structure(s) responsible for the pain and sub-optimal function (4). Orthopaedic shoulder tests fall into a number of different categories. Tests have been proposed to identify instability; such as the load and shift, sulcus and provocation tests (5).The Neer impingement sign (6), the Hawkins test (7) and the internal rotation resistance strength test (8) have been proposed to assess impingement. Clinicians identify labral pathology utilising tests such as the; O’Brien active compression test (9) the Crank test (10) and Kim test (11). Recommendations to identify rotator cuff and biceps tendon pathology include; Speed’s test (4), Yergason’s test (4) and Empty can test (12). Clinical tests are devised by designing a clinical test to stretch, contract and / or compress a specific shoulder tissue. The diagnostic accuracy of the test is then determined by comparing the clinical outcome with a ‘gold’ standard comparison, such as; radiography, ultrasound scan, magnetic resonance imaging, computed tomography and direct observation such as during open or arthroscopic surgery. The gold standard tests involve observation of structural pathology, and it is this structural pathology which is considered to be the source of symptoms. In the shoulder, structural pathology such as; rotator cuff tendinopathy, bursal effusion, partial and full thickness rotator cuff tears, labral lesions and degenerative joint changes are considered to generate symptoms and the symptoms produced during the clinical tests are compared against these changes. For example weakness and pain during the empty can test becomes diagnostic for supraspinatus pathology (tendinosis through to full thickness tear) if an US or MRI scan demonstrates structural failure. A true positive occurs when the gold standard test is positive (ie observable rotator cuff tear) and the clinical test is positive (ie pain and weakness). A true negative is when the clinical test is negative (ie no pain and weakness) and the gold standard test (ie MRI and US) does not demonstrate any structural failure. This process allows for the construction of the classic 2x2 table used to determine diagnostic accuracy (Figure 1).
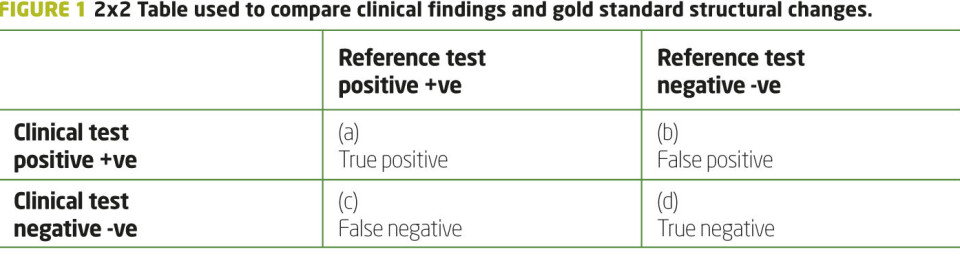
In this example if a patient presents with a painful shoulder and a test for a labral tear is positive and an MRI demonstrates a labral tear this would be a true positive. If the clinical test does not produce symptoms and an MRI demonstrates no labral pathology then this is a true negative. Clinical tests that produce only true positive and true negative results provide clinicians with considerable diagnostic confidence to enable clinical reasoning, treatment planning and patient education. However, situations occur when the clinical test is negative and the diagnostic reference test is positive, and the clinical test is positive and the diagnostic reference test is negative. These results are respectively known as false negatives and false positives. For a clinical assessment procedure to be of clinical value to identify symptomatic pathology in only one structure both the sensitivity of the test (true positive / true positive and false negative) and specificity of a test (true negative / true negative and false positive) both must be as close to 100% as possible (13). This can only occur if the clinical test assesses only 1 structure and the gold standard reference tests only demonstrate structural pathology when symptoms are present.
Reproduction of symptoms
If the sensitivity is high (ie close to 100%) but the specificity is low, then the clinician will be able to reproduce symptoms but in reality will not know which structure is causing the symptoms. Unfortunately this is the case for the majority of tests designed to test for impingement and rotator cuff pathology. The clinical tests often reproduce the symptoms of pain and weakness but frequently the reference tests are negative, and equally the clinical tests are negative and the reference tests are positive (14-17). Sometimes the specificity of a test may only be 50% (16, 17) which would not allow the clinician to develop an informed opinion as to where the symptoms were coming from. Calis et al (18) reported a sensitivity of 88.7% and a specificity of 30.5% for the Neer impingement sign. Litaker et al (19) reported values of 97.4% and 9.0% for the same test. Calis et al (18) reported sensitivity and specificity values of 92.1% and 25% for the Hawkin’s test. These figures clearly question the ability to arrive at a definitive diagnosis. Hegedus et al (20) have recently published a comprehensive review investigating clinical shoulder tests. They concluded that the use of any single shoulder orthopaedic tests to make a conclusive diagnosis is questionable.
If diabetes is suspected, it is conceivable that both clinicians and patients might be reluctant to commence insulin therapy if a blood test was only 50% accurate in detecting diabetes as the cause of the presenting symptoms. However many patients are being referred for surgery (subacromial decompression and rotator cuff repair) on the basis of clinical tests that cannot definitively confirm a diagnosis and imaging tests that might demonstrate structural pathology but the structural changes may be entirely asymptomatic (15, 21-26).
There are many reasons why the clinical orthopaedic tests for the shoulder are incapable of isolating individual structures. These include; (i) rotator cuff tendons that are not individual units but attach to other tendons and tissues such as ligaments and capsules (27, 28), and (ii) the presence of up to 12 bursae around the shoulder (29) that are capable of generating pain (30). These structures may be stretched and / or compressed in all the shoulder orthopaedic tests. In addition to this, weakness may not be true weakness but be due to pain inhibition (31, 32). It is not known why structural change may not be symptomatic but with studies reporting that up to 50% or more of people without symptoms may have structural change (21, 22, 24, 25), imaging cannot inform a clinician conclusively where the symptoms are emanating from. These issues have recently been explored in detail (15, 26).
Currently it appears that the process of making a diagnosis using a combination of clinical tests supported by imaging findings will not allow a clinician to arrive at a structural diagnosis with certainty (26). This has been recognized by clinicians treating other areas of the body (33, 34).
The Shoulder Symptom Modification Procedure
With respect to the shoulder, some clinicians have recognized that making a structural diagnosis is challenging and have moved towards a symptoms modification approach (26, 35, 36). One such process is known as the Shoulder Symptom Modification Procedure (SSMP) (26). The SSMP involves a sequential process that aims at immediately identifying postures and techniques that will reduce symptoms. Initially a number of postures, movements and activities that reproduce shoulder symptoms are identified, quantified and qualified. These are patient determined and are associated with symptoms that if reduced or eliminated would make a measureable improvement to the quality of the patients life. Once identified, the first procedure is to determine the immediate effect of altering the thoracic kyphosis on the symptoms. This is either done actively or in the case of more challenging functions, such as; swimming, throwing, push ups or other complex upper limb function, tape is used to control the kyphosis (26). If this single procedure totally alleviates symptoms, treatment is instigated to reduce the kyphosis. This may be done by postural awareness exercises, strengthening exercise, stretching, thoracic mobilizations and taping. The SSMP algorithm requires each technique to be tested on 2 separate occasions to ensure the effect of any modification procedure is consistent and mechanical. If the thoracic procedure reduces symptoms by 100% on two occasions, treatment is only directed at treating this. If reducing the kyphosis makes no impact on symptoms then the next part of the algorithm is assessed. If reducing the kyphosis results in a partial reduction in symptoms, the effect of this is then added to the next part of the algorithm. The next part of the algorithm involves assessing three planes of scapular position and combinations of positions on symptoms. This may be done during weight bearing and non-weight bearing activities. The changes to scapular position are minimal and are not designed to restrict or facilitate scapular movement. They only serve to alter the starting position of the scapula and the way the scapular moves on the thorax and articulates with the humeral head. Again if this procedure alone or in combination with the thoracic procedure results in 100% reduction in symptoms on two occasions the assessment procedure is stopped and treatment commenced. If all symptoms are not resolved then the next part of the algorithm is assessed. The next component of the SSMP is to investigate the relationship between the glenoid fossa and humeral head. This component assesses the glenohumeral relationship by using up to 13 very quick procedures. Testing stops if one or a combination of techniques results in 100% reduction of symptoms (on two occasions). As with the other parts of the SSMP algorithm, techniques that are used to assess and reduce symptoms are then used to inform techniques that are used to treat. As this is patient lead, it is hoped that improved compliance results from the fact it is the patient that has identified what is helping to reduce their symptoms. The final component of the Shoulder Symptom Modification procedure is determining the effect of neuromodulation procedures on shoulder symptoms. This involves, manual therapy, taping and soft tissue based techniques. If all the symptoms are eliminated by one part or a combination of components of the SSMP then no further investigation is required. If the SSMP fails to reduce any symptoms (as will happen with frozen shoulder) another care pathway is instigated. If the SSMP partially reduces symptoms then a determination of the reasons for the remaining symptoms is made and appropriate treatment instigated. Common reasons for this are a concomitant rotator cuff and / or biceps tendinopathy. In addition to using the componenets of the SSMP that reduced symptoms, alternative treatment is instigated respecting the stage of the tendinopathy (37). It is essential that prior to applying the SSMP other causes of pain and symptoms such as sinister pathology / red flags are carefully and thoroughly screened for (38). If the patient fails to respond, then an appropriate onward referral is mandatory.
Conclusions
The SSMP has been advocated due to the clinical dilemma of making a definitive structural diagnosis. The reliability of the procedure is currently being tested in intra- and inter-tester reliability studies and its ability to inform management will also be subject to future research. In addition to shoulder management approaches such as the Shoulder Symptom Modification Procedure (26), effort is required to develop ways to improve methods of making a structural diagnosis through enhanced clinical and imaging procedures.
References
1. Brox JI. Regional musculoskeletal conditions: shoulder pain. Best Pract Res Clin Rheumatol. 2003;17(1):33-56.
2. van der Heijden GJ. Shoulder disorders: a state-of-the-art review. Baillieres Clin Rheumatol. 1999;13(2):287-309.
3. Taylor W. Musculoskeletal pain in the adult New Zealand population: prevalence and impact. N Z Med J. 2005;118(1221):U1629.
4. Magee D. Orthopedic Physical Assessment. 3rd ed. Philadelphia: WB Saunders Co; 1997.
5. Tzannes A, Paxinos A, Callanan M, Murrell GA. An assessment of the interexaminer reliability of tests for shoulder instability. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2004;13(1):18-23. Epub 2004/01/22.
6. Neer CS, 2nd. Impingement lesions. Clinical orthopaedics and related research. 1983(173):70-7.
7. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. The American journal of sports medicine. 1980;8(3):151-8.
8. Zaslav KR. Internal rotation resistance strength test: a new diagnostic test to differentiate intra-articular pathology from outlet (Neer) impingement syndrome in the shoulder. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2001;10(1):23-7.
9. O'Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. The American journal of sports medicine. 1998;26(5):610-3.
10. Liu SH, Henry MH, Nuccion SL. A prospective evaluation of a new physical examination in predicting glenoid labral tears. The American journal of sports medicine. 1996;24(6):721-5.
11. Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel test for posteroinferior labral lesion of the shoulder--a comparison to the jerk test. The American journal of sports medicine. 2005;33(8):1188-92.
12. Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. The American journal of sports medicine. 1982;10(6):336-9.
13. Sackett D, Straus S, Richardson W, Rosenberg W, Haynes R. Evidence-based medicine. How to teach and practice EBM. 2 ed. Edinburgh: Churchill Livingstone; 2000.
14. Lewis JS. Rotator cuff tendinopathy / subacromial impingement syndrome: Is it time for a new method of assessment? British journal of sports medicine. 2008.
15. Lewis JS. Subacromial impingement syndrome: A musculoskeletal condition or a clinical illusion? Physical Therapy Review. 2011;16(5):388-98.
16. Lewis JS, Tennent TD. How effective are diagnostic tests for the assessment of rotator cuff disease of the shoulder? In: MacAuley D, Best TM, editors. Evidenced Based Sports Medicine. 2nd ed. London: Blackwell Publishing; 2007.
17. Hegedus EJ, Goode A, Campbell S, Morin A, Tamaddoni M, Moorman CT, 3rd, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. British journal of sports medicine. 2008;42(2):80-92; discussion
18. Calis M, Akgun K, Birtane M, Karacan I, Calis H, Tuzun F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Annals of the rheumatic diseases. 2000;59(1):44-7.
19. Litaker D, Pioro M, El Bilbeisi H, Brems J. Returning to the bedside: using the history and physical examination to identify rotator cuff tears. J Am Geriatr Soc. 2000;48(12):1633-7.
20. Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. British journal of sports medicine. 2012;46(14):964-78. Epub 2012/07/10.
21. Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77(2):296-8.
22. Frost P, Andersen JH, Lundorf E. Is supraspinatus pathology as defined by magnetic resonance imaging associated with clinical sign of shoulder impingement? Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 1999;8(6):565-8.
23. Connor PM, Banks DM, Tyson AB, Coumas JS, D'Alessandro DF. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: a 5-year follow-up study. The American journal of sports medicine. 2003;31(5):724-7.
24. Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77(1):10-5.
25. Miniaci A, Mascia AT, Salonen DC, Becker EJ. Magnetic resonance imaging of the shoulder in asymptomatic professional baseball pitchers. The American journal of sports medicine. 2002;30(1):66-73.
26. Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment? British journal of sports medicine. 2009;43(4):259-64.
27. Clark J, Sidles JA, Matsen FA. The relationship of the glenohumeral joint capsule to the rotator cuff. Clinical orthopaedics and related research. 1990(254):29-34.
28. Clark JM, Harryman DT, 2nd. Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74(5):713-25.
29. Codman E. The Shoulder: Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Boston: Thomas Todd Company; 1934.
30. Gotoh M, Hamada K, Yamakawa H, Inoue A, Fukuda H. Increased substance P in subacromial bursa and shoulder pain in rotator cuff diseases. J Orthop Res. 1998;16(5):618-21.
31. Steenbrink F, de Groot JH, Veeger HE, Meskers CG, van de Sande MA, Rozing PM. Pathological muscle activation patterns in patients with massive rotator cuff tears, with and without subacromial anaesthetics. Manual therapy. 2006;11(3):231-7.
32. Wassinger CA, Sole G, Osborne H. The role of experimentally-induced subacromial pain on shoulder strength and throwing accuracy. Manual therapy. 2012;17(5):411-5. Epub 2012/04/17.
33. O'Sullivan P. It's time for change with the management of non-specific chronic low back pain. British journal of sports medicine. 2012;46(4):224-7. Epub 2011/08/09.
34. Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. The Journal of orthopaedic and sports physical therapy. 2007;37(9):541-50. Epub 2007/10/18.
35. Mulligan BR. Manual Therapy “Nags”, “Snags”, “MWMs” etc. 4th ed. New Zealand: Plane View Services; 1999.
36. McKenzie R, Watson G, Lindsay R. Treat your own shoulder. New Zealand: Spinal Publications New Zealand Limited; 2009.
37. Lewis JS. Rotator cuff tendinopathy: a model for the continuum of pathology and related management. British journal of sports medicine. 2010;44(13):918-23.
38. Greenhalgh S, Self J. Red flags: A guide to identifying serious pathology of the spine. Edinburgh: Churchill Livingstone Elsevie; 2006.
Other relevant resources:
Download copies of the Shoulder Symptom Modification Procedure at www.LondonShoulderClinic.com
Podcast: Prof Jeremy Lewis: Rotator cuff tendinopathies.BMJ Group Podcasts http://podcasts.bmj.com/bjsm/
Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment? British Journal of Sports Medicine. 2009;43(4):259-64. http://bjsm.bmj.com/content/43/4/259.long
Lewis JS. Rotator cuff tendinopathy: a model for the continuum of pathology and related management. British Journal of Sports Medicine. 2010;44(13):918-23. http://bjsm.bmj.com/content/44/13/918.full.pdf+html
Lewis JS. Subacromial impingement syndrome: A musculoskeletal condition or a clinical illusion? Physical Therapy Review. 2011;16(5):388-98. http://dx.doi.org/10.1179/1743288X11Y.0000000027






















